Archive for January 2013
Central Cord Syndrome
Central Cord Syndrome (CCS) is an incomplete injury to the cervical cord resulting in more extensive motor weakness in the upper extremities than the lower extremities. The mechanism of injury occurs from a hyperextension injury with pre-existent osteophytic (abnormal bony outgrowth) spurs, without damage to the vertebral column.
Mechanism and Causes of Injury
CCS occurs typically in patients with hyperextension injuries where the spinal cord is squeezed or pinched between anterior cervical spondylotic bone spurs and the posterior intraspinal canal ligament, the ligamentum flavum. The ligamentum flavum is a strong ligament that connects the laminae of the vertebrae. It serves to protect the neural elements and the spinal cord and stabilize the spine so that excessive motion between the vertebral bodies does not occur.
The injury occurs as a result of anterior and posterior compression of the spinal cord, leading to edema, hemorrhage or ischemia to the central portion of the spinal cord. The site of most injuries is in the mid-to-lower cervical cord. Due to the anatomical lamination of the corticospinal tract with the arm fibers medially, and the leg fibers laterally, the arms are affected more so than the legs, resulting in a disproportionate motor impairment.
Symptoms
Patients are typically left with motor weakness of the upper extremities and lesser involvement of the lower extremities. A varying degree of sensory loss below the level of the lesion and bladder symptoms (urinary retention) may both occur.
Incidence
This syndrome more commonly affects patients age 50 and older who have sustained a cervical hyperextension injury.
CCS may occur in patients of any age and is seen in athletes who present with not only hyperextension injuries to their neck but associated ruptured disc(s) with anterior cord compression.
CCS affects males more frequently than females.
Diagnosis
Evaluation of the patient includes a complete history, a thorough neurological exam, MRI and CT of the cervical spine, and cervical spine x-rays including supervised flexion and extension x-rays.
- Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology; can show direct evidence of spinal cord impingement from bone, disc, or hematoma.
- Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads x-rays; can show the shape and size of the spinal canal, its contents, and the structures around it.
- X-ray: Application of radiation to produce a film or picture of a part of the body can show the structure of the vertebrae and the outline of the joints. X-rays of the spine delineate fractures and dislocations, as well as the degree and extent of spondylitic changes. Flexion/extension views assist in evaluation of ligamentous stability.
Surgical Treatment
Acute surgical intervention is not usually necessary unless there is significant cord compression. Prior to the CT-MRI era, surgical intervention was thought to be more harmful because of the risk of injuring a swollen cervical cord and worsening the deficit. However, with advanced imaging technology such as CT and MRI, patients with compression of the spinal cord secondary to traumatic herniated discs and other lesions can be quickly diagnosed and surgically decompressed. In cases with anterior bony ridges and spinal canal narrowing secondary to ligamentous thickening and or stenosis, acute surgery is usually not performed until the patient has made maximum recovery. Reassessment at that time may lead to surgery depending on the underlying cause. If there is significant motor weakness after a period of recovery, or neurological deterioration or spinal instability, then surgical intervention may be considered.
Nonsurgical Treatment
Nonsurgical treatment consists of immobilization of the neck with a cervical orthosis, steroids unless contraindicated, and rehabilitation with physical and occupational therapy.
Outcome
Many patients with CCS make spontaneous recovery of motor function while others experience considerable recovery in the first six weeks post injury.
If the underlying cause is edema, recovery may occur relatively soon after an initial phase of motor paralysis or pareses. Leg function usually returns first, followed by bladder control and then arm function. Hand movement and finger dexterity improves last. If the central lesion is caused by hemorrhage or ischemia, then recovery is less likely and the prognosis is more devastating.
The prognosis for CCS in younger patients is favorable. Within a short time, a majority of younger patients recover and regain the ability to ambulate and perform daily living activities. However, in elderly patients the prognosis is not as favorable, with or without surgical intervention.
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us
Carpal Tunnel Syndrome, CTS
Carpal tunnel syndrome is a common problem that affects the use of your hand, and is caused by compression of the median nerve at the wrist. It most often occurs when the median nerve in the wrist becomes inflamed after being aggravated by repetitive movements such as typing on a computer keyboard or playing the piano. It also seems to affect professional artists fairly commonly – in particular, sculptors and printmakers.
The “carpal tunnel” is formed by the bones, tendons and ligaments that surround the median nerve. Since the median nerve supplies sensation to the thumb, index and middle finger, and part of the ring finger, and provides motion to the muscles of the thumb and hand, you might notice numbness and weakness in these areas.
Common Symptoms
- Hand and wrist pain
- A burning sensation in the middle and index fingers
- Thumb and finger numbness
- An electric-like shock through the wrist and hand
Thesesymptoms are often exaggerated when the wrist is bent forward. This numbness or pain may be worse at night, and may actually keep you awake. During the day, it may occur more often when you are participating in activities that involve bending of your wrist.
Common Causes of Carpal Tunnel Syndrome
Diseases or conditions that may increase your chances of developing carpal tunnel syndrome include pregnancy, diabetes, menopause, broken or dislocated bones in the wrist, and obesity. Additional causes include repetitive and forceful grasping with the hands, bending of the wrist, and arthritis.
Any repetitive motions that cause significant swelling, thickening or irritation of membranes around the tendons in the carpal tunnel can result in pressure on the median nerve, disrupting transmission of sensations from the hand up to the arm and to the central nervous system.
Diagnosing Carpal Tunnel Syndrome
It is important to seek medical assistance when you first notice persistent symptoms. Do not wait for the pain to become intolerable.
Before your doctor can recommend a course of treatment, he or she will perform a thorough evaluation of your condition, including a medical history, physical examination and diagnostic tests. Your doctor will document your symptoms and ask about the extent to which these symptoms affect your daily living. The physical examination will include an assessment of sensation, strength and reflexes in your hand.
If conservative treatment such as medication or physical therapy does not provide sufficient relief, your doctor may perform diagnostic studies to determine if surgery is an effective option. These diagnostic studies may include:
- X-ray: An x-ray will show the bones of the wrist and determine if any abnormalities may be contributing to carpal tunnel syndrome or another disorder.
- Electromyogram and Nerve Conduction Studies (EMG/NCS): These tests primarily study how the nerves and muscles are working together. They measure the electrical impulse along nerve roots, peripheral nerves and muscle tissue.
Conservative (Nonsurgical) Treatments
The main purpose of conservative treatment is to reduce or eliminate repetitive injury to the median nerve. In some cases, carpal tunnel syndrome can be treated by immobilizing the wrist in a splint to minimize or stop pressure on the nerves. If that does not work, patients are sometimes prescribed anti-inflammatory medications or cortisone injections in the wrist to reduce swelling. Your doctor may suggest specific types of hand and wrist exercises, which may be helpful. Treatment for carpal tunnel syndrome may include rest, the use of a wrist splint during sleep, or physical therapy. Conservative treatment methods may continue for up to eight weeks.
Only a small percentage of patients require surgery. Factors leading to surgery include the presence of persistent neurological symptoms and lack of response to conservative treatment.
If you experience severe pain that cannot be relieved through rest, rehabilitation or nonsurgical treatment, you may be a candidate for one of several surgical procedures that can be performed to relieve pressure on the median nerve. The most common procedure is called carpal tunnel release, which can be performed using an open incision or endoscopic techniques.
The open incision procedure or carpal tunnel release, involves the doctor opening your wrist and cutting the ligament at the bottom of the wrist to relieve pressure. The endoscopic carpal tunnel release procedure involves making a smaller incision and using a miniaturized camera to assist the neurosurgeon in viewing the carpal tunnel. The possibility of nerve injury is slightly higher with endoscopic surgery, but the patient’s recovery and return to work is quicker.
After surgery, a dressing will be applied to your hand. You should leave this secured in place until your first office visit following surgery. You may need bandages on one or both wrists depending on your surgery. If this is the case, you may require extra assistance at home with everyday activities. Your stitches can be removed about 10-14 days after surgery. Make sure you avoid repetitive use of the hand for four weeks after surgery and avoid getting the stitches wet. You will notice that the pain and numbness begins to improve after surgery, but you may have tenderness in the area of the incision for several months.
Recurrence of symptoms after surgery for carpal tunnel syndrome is rare, occurring in less than 5 percent of patients. A majority of patients recover completely. To avoid injuring yourself again, it may help to change the way you perform repetitive movements, the frequency with which you perform the movements, and the amount of time you rest between periods when you must perform these movements.
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us https://www.becomepainfree.com/
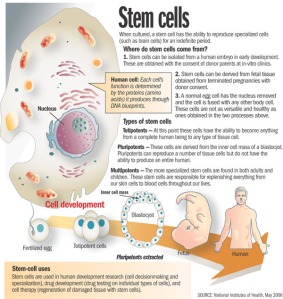
Regenerative Medicine
Administering undifferentiated stem cells to an injured disc has made adult stem cell regenerative medicine in spine a reality. Adult stem cell regenerative medicine holds the promise of stabilizing or even reversing the degenerative changes associated with aging or following traumatic injury. Current clinical use of stem cells is very limited, in part by the cumbersome approval process. The use of concentrated bone marrow aspirate (BMC) as a “stem cell” preparation is currently the simplest and safest way of utilizing the regenerative potential for mesenchymal stem cells (MSCs) to promote tissue regeneration. In fact, stem cells concentrated from bone marrow have been shown to stimulate the formation of bone, cartilage, ligament and tendon, and dermal tissues.
Conservative treatment options for lumbar and cervical pain associated with discogenic disc disease (Pfirrmann Grades 3-6) are limited. Treatment options include pain medication, steroids, physical therapy, and chiropractic care. Reversal of disc pathology has not been achieved with current available treatment modalities. Failure of these nonoperative treatments may leave surgical intervention as a treatment option.
The goal of utilizing MSCs is to not only potentially provide pain relief from the painful degenerative disc, but to reverse the degenerative process. There are three methods for placing MSCs into the painful nucleus pulposus.
The use of allogeneic mesenchymal precursor cells (MPCs) is currently being evaluated as a part of an FDA Phase I clinical trial. Extracted from donors and expanded in number by tissue culture, this process isolates and grows the stem cells into pure MPCs which are injected into the nucleus pulposus. This technology does not have FDA approval.
Utilizing expanded, autologous MSCs for injection into the painful disc is the second method. Federal regulations require the approval of an Investigational New Drug application supported by prospective, randomized clinical trials for the use of expanded autologous MSCs. The FDA has not approved this technology.
The third method involves autologous point of care therapy. This technology does not require FDA approval. The patient’s own MSCs are directly injected into the nucleus pulposus of the symptomatic degenerated disc(s) using standardized two needle discography technique. This requires fluoroscopic visualization and 2-3cc of MSCs are slowly injected into the symptomatic nucleus pulposus.
There have been no complications associated with the iliac crest aspiration or disc injection. Thus far no patient in the study has undergone spine surgery following treatment. Results obtained with this technique suggest its potential clinical efficacy in the treatment of moderate to severe degenerative disc disease. These results require verification with longer follow-up and randomized prospective studies.
For more information regarding treatment options please visit our websites at http://www.becomepainfree.com
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us
Adult Stem Cell Therapy to Treat Back Pain, Stem Cell, Spine Stem Cells, Stem Cell Treatment
Adult Stem Cell Therapy that doesn’t require FDA approval to treat lumbar and cervical spine conditions resulting from injury or aging, and is also involved with an FDA clinical trial investigating the use of Adult Stem Cells.
These stem cells are autologous – they are taken from an adult patient and returned to that same patient in a concentrated form to the damaged area in a 30-minute procedure. This type of adult stem cell therapy does not require FDA approval to administer.
When it comes to stem cells, there is often a lot of mystique surrounding them. We hear from the media that we can create a human being out of a bundle of cells, which is not necessarily true. We also tend to look at embryonic stem cells as being the only type of stem cell. With these types of embryonic stem cells, one idea is to be able to create a liver or kidney in a Petri dish, which is not controllable or feasible at this point, and the work being done by the BecomePainFree.com medical group.
When we look at stem cell types, we have embryonic stem cells on one hand and adult stem cells on the other. The characteristics of each of these are not like other cells. For instance, a liver cell can divide but it will only ever be a liver cell. These stem cells, both embryonic and adult, can turn into different types of cells. The embryonic stem cells can really turn into any cell type, but adult stem cells are limited as far as the cells they can turn into. This depends upon environment or niche and what they are already programmed to become. A lot of people think there is a lot of promise with embryonic stem cells and there is, although we are not quite there yet.
We are still at the forefront of stem cell technology and embryonic stem cells in particular. With those cells, we do not have the ability to control what types of tissue they turn into. For example, we could be trying to manipulate these cells to turn into kidneys, but they might start to develop as pancreatic cells, which is troublesome. Another key with all stem cells is that they can proliferate quite a bit, usually at a higher rate than just a regular somatic cell. Although this sounds good at first glance, the issue with this, particularly with embryonic stem cells, is we cannot control that division. Hence, these cells can keep going and going without dying. In the normal bodily process, cells are programmed to die after a certain time, but these embryonic stem cells can evade that action and continue dividing, which takes on the characteristic of cancer cells. In some animal studies, an issue that keeps arising is development of tumors in some of these animals. It is difficult to predict if tumors are going to form when using some sort of embryonic stem cell treatment. This is still a scary area through which we are still trying to navigate.
However, the focus of the BecomePainFree.com medical group is on adult mesenchymal stem cells. On the whole, the media does not give a lot of attention to these kinds of stem cells, as using them avoids any kind of ethical or controversial issues. There is a great amount of research being done on adult mesenchymal stem cells, however, because they are very powerful.
First off, we can control what cell type they turn into much more easily. For example, the treatment used by the BecomePainFree.com medical group focuses on Mesenchymal precursor cells (MPC). Mesenchymal means these cells are not going to turn into any kind of blood product such as a red blood cell or white blood cell, although they are derived from bone marrow. The fact that they are precursor cells means these MPCs are only going to differentiate into one of a few cell types. They are either going to become bone cells, i.e., osteoblasts, or chondrocytes, i.e., cartilaginous tissue such that we see in intervertebral discs and joints, etc. All of that really depends on the environment in which we place these adult stem cells where it is well suited to do this. For example, we can inject these MPCs into a bone fracture, and because the cells are surrounded by bone tissue, these cells will receive signals from the surrounding cells that tell them to turn into bone. However, the cells we use will be injected into a disc or joint, and the cells composing the disc and joint tissue will signal the stem cells to develop into similar tissue. Again, there is no chance of any sort of pancreatic cell or nerve cell type spontaneously forming because we are using certain adult stem cell types, which are limited and cannot turn into anything like that. In addition, as the tissue surrounding the disc and joint is relatively avascular, there is not really any worry of these cells migrating through the blood stream to somewhere else in the body and causing any sort of problem. As far as the proliferation issue with embryonic stem cells, we have not seen this issue with adult stem cells in terms of dividing exponentially without ceasing. There is almost a preset limit to how many times these adult stem cells will divide.
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us https://www.becomepainfree.com/
Confusion about Spinal Fusion, Spine Fusion, Spine Fusion Surgery, Back Fusion Surgery, Back Surgery
Spinal Fusion is used to treat spinal instability and alleviate chronic mechanical back pain but many people are unsure of what spinal fusion actually does. Spinal fusion is surgery to permanently connect two or more vertebrae in your spine, eliminating motion between them.
Spinal fusion involves many techniques designed to mimic the normal healing process of broken bones. During spinal fusion, your surgeon places bone or a bone-like material within the space between two spinal vertebrae. Metal plates, screws and rods may be used to hold the vertebrae all together, so they can heal into one solid unit.
Because spinal fusion surgery immobilizes parts of your spine, it changes the way your spine can move. This places additional stress and strain on the vertebrae above and below the fused portion, and may increase the rate at which those areas of your spine degenerate.
BecomePainFree.com can help
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us
Laser Spine Surgery Does it Work?, Laser Spine Institute, LSI, Laser Back Surgery, Laser Spine Work
Here’s the real answer: www.becomepainfree.com can help!
A board certified typically does spine surgery and or fellowship trained spine surgeon to relieve pain and other symptoms by decreasing the pressure on a compressed nerve or by stabilizing the spine. In the case of a herniated or ruptured disc area, a discectomy may be done to remove the damaged portion of a disc in the spine; or a laminectomy may be done to remove bone spurs or other spinal growths. In cases where the spine is very unstable, a spinal fusion can be performed to secure together two or more of the vertebral bones so that they “fuse” together. These surgeries are now often performed using minimally invasive techniques that minimize damage to the surrounding tissue and allow for a faster recovery with much less blood loss. Laser spine surgery is often promoted as being minimally or even noninvasive and risk-free. However, these laser spine procedures do require incisions and the laser itself can result in many serious complications.
Laser spine surgery or Laser Back Surgery has never been studied in a controlled clinical trial to determine its effectiveness. Marketing pitches for spine surgery performed with a laser often make bold major promises of pain relief for chronic neck and back pain and a quick return to normal life; sometimes in a matter of days. What is often not clear from marketing hype is that laser spine surgery or laser back surgery done at such places as the laser spine institute does actually involve surgery. An incision is required to allow access to the spine area in need of care. A focused beam of light (laser) is then used only to remove the soft tissues over the spine. Bone and ligament are then removed in order to free the nerve from compression using small instruments. The laser in laser spine surgery or laser back surgery actually plays a very minor role in the total surgical procedure of the spine.
Lasers are certainly not new technology by any means. Lasers have been available for use in medicine since 1973. However, they have not been widely adopted as a tool to be used in spinal surgery ever. The fact is that most neurosurgeons do not use or recommend the use of lasers for any spine surgery because there are no clear benefits and there are other well-established and documented studies proving the effectiveness of more modern and established spine surgery techniques.
The Importance of a Proper Diagnosis of you Condition
It is important to have a proper diagnosis of your problem before deciding to undergo spine major surgery. Most cases of back and neck pain are muscular in origin and do not require or benefit from surgery. Unless severe pain or muscle weakness is making walking or performing daily activities extremely difficult, surgery is rarely the first line of treatment ever. Anti-inflammatory medication, physical therapy and exercise, lifestyle changes and other noninvasive treatment modalities such as therapeutic massage are often successful at resolving back and neck pain.
If conservative treatments fail to reduce back pain, then surgery may be necessary, depending on your current diagnosis. For example, if you have a herniated disk with leg or arm pain as a major symptom that hasn’t been relieved with other treatments, discectomy may be appropriate. If surgery is recommended, get a clear explanation of your diagnosis and how the surgery will help relieve your symptoms.
Traditional spine surgery has been tested in numerous clinical trials. The major vast majority of patients who undergo discectomy for treatment of a herniated disc experienced relief from pain and other symptoms. In elderly patients diagnosed with spinal stenosis, laminectomy is also a highly effectively procedure. Very few neurosurgeons regard laser spine surgery as a viable alternative to conventional spine surgery techniques. BecomePainFree spine surgeons do not use or recommend laser spine surgery or laser back surgery such as the ones done at the laser spine institute.
Mayo Clinic Opinion on Laser Spine Surgery
https://www.becomepainfree.com/ can Help!
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us