Posts Tagged ‘invasive spine surgery’
The 5 things you should know about chronic pain from BecomePainFree.com
Only sufferers of chronic pain know the implications of pain in every aspect of life. Family members and friends of someone with chronic pain may sympathize to some extent, but it’s difficult to truly understand how chronic pain affects someone. If you have a friend or family member suffering from chronic pain — whether caused by an accident or injury, or another health condition such asfibromyalgia — use these tips to understanding chronic pain to help you be most supportive to your loved one.
1.Don’t pass chronic pain off as “all in your head.” People who suffer from chronic pain are rarely fabricating or exaggerating their symptoms. Conditions causing chronic pain can make an individual truly miserable. Many cases of chronic pain are difficult to diagnose, and thus management and treatment is far more challenging than in cases of acute pain, where the source of pain is easily diagnosed.
2.Chronic pain is different from acute pain. Acute pain lasts for a brief period of time, perhaps following an injury or accident. Chronic pain, on the other hand, is persistent and can even be permanent. We have all felt acute pain at some point in time, but only those with chronic pain know what it is to be in pain constantly.
3.Chronic pain may be caused by or the cause of other health conditions. Difficulty sleeping and depression are two conditions that often plague sufferers of chronic pain. Chronic pain can create a vicious cycle for the sufferer, for example: chronic pain leads to sleep disturbances, whereas lack of sleep can exacerbate chronic pain. The same is true of depression; it can be caused by or the cause of some chronic pain symptoms.
4.Every person’s pain is different. We all experience and express pain differently. Some people may be more tolerant of pain in specific parts of the body, while other people may express discomfort with pain in the same area or caused by the same condition.
5.Chronic pain is emotionally exhausting. Imagine that you are in pain or don’t feel good for months or years on end, with no relief. Constant pain wears on the emotions and can lead to depression and anger. Treatment for chronic pain often means treating each symptom and effect of that pain, including mental health issues such as depression.
Chronic pain is a lonely condition. If someone you know or love is suffering from chronic pain, don’t try to compare their pain to your own experiences, or assume their pain is all made up. Rather, offer your care and support. Be willing to listen when they need to talk and supportive throughout treatment programs.
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us
Regenerative Medicine
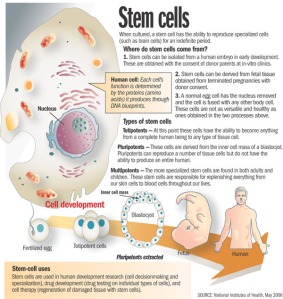
Administering undifferentiated stem cells to an injured disc has made adult stem cell regenerative medicine in spine a reality. Adult stem cell regenerative medicine holds the promise of stabilizing or even reversing the degenerative changes associated with aging or following traumatic injury. Current clinical use of stem cells is very limited, in part by the cumbersome approval process. The use of concentrated bone marrow aspirate (BMC) as a “stem cell” preparation is currently the simplest and safest way of utilizing the regenerative potential for mesenchymal stem cells (MSCs) to promote tissue regeneration. In fact, stem cells concentrated from bone marrow have been shown to stimulate the formation of bone, cartilage, ligament and tendon, and dermal tissues.
Conservative treatment options for lumbar and cervical pain associated with discogenic disc disease (Pfirrmann Grades 3-6) are limited. Treatment options include pain medication, steroids, physical therapy, and chiropractic care. Reversal of disc pathology has not been achieved with current available treatment modalities. Failure of these nonoperative treatments may leave surgical intervention as a treatment option.
The goal of utilizing MSCs is to not only potentially provide pain relief from the painful degenerative disc, but to reverse the degenerative process. There are three methods for placing MSCs into the painful nucleus pulposus.
The use of allogeneic mesenchymal precursor cells (MPCs) is currently being evaluated as a part of an FDA Phase I clinical trial. Extracted from donors and expanded in number by tissue culture, this process isolates and grows the stem cells into pure MPCs which are injected into the nucleus pulposus. This technology does not have FDA approval.
Utilizing expanded, autologous MSCs for injection into the painful disc is the second method. Federal regulations require the approval of an Investigational New Drug application supported by prospective, randomized clinical trials for the use of expanded autologous MSCs. The FDA has not approved this technology.
The third method involves autologous point of care therapy. This technology does not require FDA approval. The patient’s own MSCs are directly injected into the nucleus pulposus of the symptomatic degenerated disc(s) using standardized two needle discography technique. This requires fluoroscopic visualization and 2-3cc of MSCs are slowly injected into the symptomatic nucleus pulposus.
There have been no complications associated with the iliac crest aspiration or disc injection. Thus far no patient in the study has undergone spine surgery following treatment. Results obtained with this technique suggest its potential clinical efficacy in the treatment of moderate to severe degenerative disc disease. These results require verification with longer follow-up and randomized prospective studies.
For more information regarding treatment options please visit our websites at http://www.becomepainfree.com
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us
Adult Stem Cell Therapy to Treat Back Pain, Stem Cell, Spine Stem Cells, Stem Cell Treatment
Adult Stem Cell Therapy that doesn’t require FDA approval to treat lumbar and cervical spine conditions resulting from injury or aging, and is also involved with an FDA clinical trial investigating the use of Adult Stem Cells.
These stem cells are autologous – they are taken from an adult patient and returned to that same patient in a concentrated form to the damaged area in a 30-minute procedure. This type of adult stem cell therapy does not require FDA approval to administer.
When it comes to stem cells, there is often a lot of mystique surrounding them. We hear from the media that we can create a human being out of a bundle of cells, which is not necessarily true. We also tend to look at embryonic stem cells as being the only type of stem cell. With these types of embryonic stem cells, one idea is to be able to create a liver or kidney in a Petri dish, which is not controllable or feasible at this point, and the work being done by the BecomePainFree.com medical group.
When we look at stem cell types, we have embryonic stem cells on one hand and adult stem cells on the other. The characteristics of each of these are not like other cells. For instance, a liver cell can divide but it will only ever be a liver cell. These stem cells, both embryonic and adult, can turn into different types of cells. The embryonic stem cells can really turn into any cell type, but adult stem cells are limited as far as the cells they can turn into. This depends upon environment or niche and what they are already programmed to become. A lot of people think there is a lot of promise with embryonic stem cells and there is, although we are not quite there yet.
We are still at the forefront of stem cell technology and embryonic stem cells in particular. With those cells, we do not have the ability to control what types of tissue they turn into. For example, we could be trying to manipulate these cells to turn into kidneys, but they might start to develop as pancreatic cells, which is troublesome. Another key with all stem cells is that they can proliferate quite a bit, usually at a higher rate than just a regular somatic cell. Although this sounds good at first glance, the issue with this, particularly with embryonic stem cells, is we cannot control that division. Hence, these cells can keep going and going without dying. In the normal bodily process, cells are programmed to die after a certain time, but these embryonic stem cells can evade that action and continue dividing, which takes on the characteristic of cancer cells. In some animal studies, an issue that keeps arising is development of tumors in some of these animals. It is difficult to predict if tumors are going to form when using some sort of embryonic stem cell treatment. This is still a scary area through which we are still trying to navigate.
However, the focus of the BecomePainFree.com medical group is on adult mesenchymal stem cells. On the whole, the media does not give a lot of attention to these kinds of stem cells, as using them avoids any kind of ethical or controversial issues. There is a great amount of research being done on adult mesenchymal stem cells, however, because they are very powerful.
First off, we can control what cell type they turn into much more easily. For example, the treatment used by the BecomePainFree.com medical group focuses on Mesenchymal precursor cells (MPC). Mesenchymal means these cells are not going to turn into any kind of blood product such as a red blood cell or white blood cell, although they are derived from bone marrow. The fact that they are precursor cells means these MPCs are only going to differentiate into one of a few cell types. They are either going to become bone cells, i.e., osteoblasts, or chondrocytes, i.e., cartilaginous tissue such that we see in intervertebral discs and joints, etc. All of that really depends on the environment in which we place these adult stem cells where it is well suited to do this. For example, we can inject these MPCs into a bone fracture, and because the cells are surrounded by bone tissue, these cells will receive signals from the surrounding cells that tell them to turn into bone. However, the cells we use will be injected into a disc or joint, and the cells composing the disc and joint tissue will signal the stem cells to develop into similar tissue. Again, there is no chance of any sort of pancreatic cell or nerve cell type spontaneously forming because we are using certain adult stem cell types, which are limited and cannot turn into anything like that. In addition, as the tissue surrounding the disc and joint is relatively avascular, there is not really any worry of these cells migrating through the blood stream to somewhere else in the body and causing any sort of problem. As far as the proliferation issue with embryonic stem cells, we have not seen this issue with adult stem cells in terms of dividing exponentially without ceasing. There is almost a preset limit to how many times these adult stem cells will divide.
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us https://www.becomepainfree.com/
Confusion about Spinal Fusion, Spine Fusion, Spine Fusion Surgery, Back Fusion Surgery, Back Surgery
Spinal Fusion is used to treat spinal instability and alleviate chronic mechanical back pain but many people are unsure of what spinal fusion actually does. Spinal fusion is surgery to permanently connect two or more vertebrae in your spine, eliminating motion between them.
Spinal fusion involves many techniques designed to mimic the normal healing process of broken bones. During spinal fusion, your surgeon places bone or a bone-like material within the space between two spinal vertebrae. Metal plates, screws and rods may be used to hold the vertebrae all together, so they can heal into one solid unit.
Because spinal fusion surgery immobilizes parts of your spine, it changes the way your spine can move. This places additional stress and strain on the vertebrae above and below the fused portion, and may increase the rate at which those areas of your spine degenerate.
BecomePainFree.com can help
Become Pain Free | Pain Specialist in Texas
Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us
Minimally Invasive Stabilization (MIS), Cervical Spine Anterior Cervical Discectomy and Stabilization (ACDS)
Anterior Cervical Discectomy and Stabilization (ACDS) is a type of minimally invasive fusion surgery that may be helpful in treating the following conditions within the cervical (neck) spine presented by BecomePainFree:
About ACDS
The ACDS procedure is designed to relieve neck pain by removing your painful disc material and bone spurs. During the ACDS procedure, the damaged disc is removed and implants are inserted to help stabilize your bones.
Like the other types of minimally invasive surgery at BecomePainFree.com, ACDS is performed through a small incision with the use of a surgical telescope. This approach eliminates the need to cut through muscle and involves minimal soft tissue damage, resulting in a quicker recovery for most patients.
Through a small incision, the surgeon will make a tunnel to the spine through the front area of the neck by moving aside muscles so that the bony vertebrae and discs can be seen. With the aid of a fluoroscope (a special X-ray), the surgeon will remove the disc and the remaining disc material. Next, open disc space is prepared for the bone graft stabilization or the artificial disc replacement. Allograft bone, or bone taken from your hip area, is used to complete the reconstruction and is then stabilized with a small titanium plate. Once that is complete, the incision is closed and the patient is on their way to postoperative recovery.
Call our group today Call Us: (214) 396-3647 | (888) 373-3720 Fax #: (888 )238-9155 | E-mail Us
https://www.becomepainfree.com/